_Wide.png)
Chiesi has been developing medicines to treat respiratory disease for more than 30 years. Thanks to modern treatments, patients with asthma or chronic obstructive pulmonary disease (COPD) are able to live more active lives with greater self-confidence. After all, to breathe is to live.
Asthma is one of the most common chronic diseases found in children and young people, although the number of adults and older people being diagnosed is also on the rise. In Germany, around 8 million people suffer from asthma, approx. 10-15% children and approx. 5-7% adults.[1] The WHO estimates that there are around 340 million asthmatics worldwide.[2]
As a chronic inflammatory disease involving extreme hypersensitivity of the airways, the typical symptoms of asthma are recurrent and sudden, including shortness of breath, coughing, wheezing and a tight feeling in the chest. These symptoms often arise at night and in the early hours of the morning, and vary widely depending on the severity of the disease.
Apart from a genetic predisposition, asthma can have a wide variety of causes that can result in swelling of the mucous membranes, narrowing of the airways and increased mucus production.
We differentiate between allergic and non-allergic asthma.
The most common triggers for allergic asthma, which is mainly diagnosed in children and young people, are pollen, food components, animal hair and mite faeces.
Non-allergic asthma, which mainly occurs in adults, can be triggered by non-specific irritants such as cold air, although environmental pollution, cigarette smoke and viral respiratory infections also play an important role.
In addition to these two types, there are also mixed forms of asthma that cannot be clearly designated, drug-induced asthma (e.g. caused by pain medications such as acetylsalicylic acid) and exercise-induced asthma.
Risk factors such as smoking and obesity also encourage the development of asthma.
Find the most important facts about asthma and further information on our website asthma-alltag.de.
The pollen count calendar gives you an overview of the months in which pollen is flying and includes a guide to breathing difficulties.
Download the pollen calendar here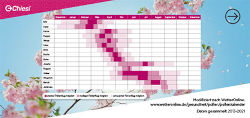
Chronic obstructive pulmonary disease, or COPD, is one of the most common diseases. Around three million people in Germany live with a diagnosis of COPD.[1]
Men are affected more frequently (over 15%) than women (just under 12%).[2] In the next few years, the increased consumption of tobacco – especially amongst females – as well as more polluted indoor air due to cooking and heating in developing countries is expected to produce another rise in the number of sufferers around the world. In statistics regarding the most common causes of death, COPD is currently ranked fourth.[3]
The umbrella term “chronic obstructive pulmonary disease” covers a number of lung diseases. These include chronic bronchitis, a very common disease that is defined as “coughing and production of sputum on most days for at least three months in two consecutive years” (Source: WHO). Chronic bronchitis often progresses to become chronic obstructive bronchitis, which in a large number of cases is related to lung emphysema, in which there is hyperinflation of the lungs.
The classic COPD symptoms are:
These symptoms usually emerge gradually over time.
Risk factors for developing COPD include long-term tobacco smoking. Around 90% of those diagnosed with COPD are smokers or have smoked in the past. Environmental factors and genetic predispositions are increasingly being discussed as risk factors.
For asthma
Today, thanks to modern medicine, asthma is easy to treat and patients are able to live their lives with few to no symptoms.
As well as avoiding disease triggers (as far as is possible in day-to-day life), therapy with inhalation drugs (e.g. corticosteroids or beta-agonists) is an important pillar in the treatment of asthma.
For COPD
Treatment of chronic obstructive pulmonary disease includes the strict avoidance of trigger factors (e.g. abstaining from smoking tobacco), exercise and respiratory therapies as well as drug-based therapy. As in asthma, this includes inhalation therapy using so-called bronchodilators (anti-cholinergic drugs and/or beta-2 sympathetic agonists) that widen the airways and so make it easier to breathe. Corticosteroids are used to counteract inflammation in the airways. Both groups of medications are also used in combination by way of a metred-dose or powder inhaler.
In the most severe cases, e.g. respiratory distress (inadequate breathing resulting in a lack of oxygen supply to the body), treatments such as oxygen delivered via a nasal tube can be used. Endoscopic or surgical interventions (lung valves, lung transplants) can be potential treatment options for some patients.
Today and tomorrow
We want to offer patients more than just medication. We also want to provide them with helpful information regarding modern, long-term treatments. We want to support those affected in living a life with few to no symptoms – even when taking part in sports or travelling, from spring right through to winter.
Chiesi will continue to conduct research into respiratory diseases in future to seek out new ways of helping patients. We are also working on new therapy solutions so that patients are better able to inhale the medication, and so that it can be optimally absorbed by the body.
The medications used in this area counteract the narrowing of the airways and so alleviate respiratory distress whilst also reducing inflammation in the bronchial tubes.
You can find tips for living with asthma and everything you need to know about your condition at asthma-alltag.de.
To find out how you can get a better grip on your “COPD” and improve your quality of life, visit copd-alltag.de.